Mon-Fri: 8:30a.m.-5:30p.m. | Sat: 9a.m.-12p.m. | Sun. & Major Holidays: Closed
Patient Resources
Get Healthy!
Suicides Among U.S. Veterans Jumped 10-Fold in Decades After 9/11
- August 28, 2023
- Steven Reinberg
- HealthDay Reporter
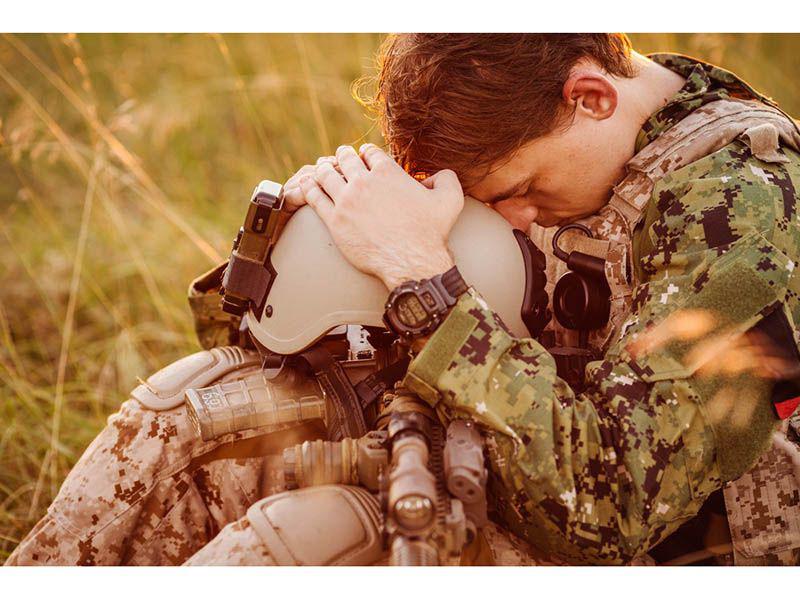
Suicide has become an urgent issue among American military veterans, with rates increasing by more than 10 times in nearly two decades, a new study reveals.
"Suicide rates for post-9/11 veterans have steadily increased over the last 15 years and at a much faster pace than the total U.S. population, and post-9/11 veterans with TBI [traumatic brain injuries] have a significantly higher suicide rate than veterans without TBI," said lead researcher Jeffrey Howard, from the department of public health at the University of Texas at San Antonio.
In fact, the suicide rate for those with a TBI was 56% higher than among veterans who didn't suffer a TBI, the researchers found.
Exposure to TBI, even a mild one, is associated with severe long-term health risks, including suicide, Howard noted.
"It used to be believed that once initial symptoms of a mild TBI resolved, the patient was healed and there were no long-term health impacts, but as we are compiling longer-term follow-up data on these patients a different picture is emerging," Howard said.
These data suggest that closer and longer-term monitoring of patients with TBIs may be needed, he explained.
"In addition to the clinical implications, the data point to the need for a more holistic approach to ensuring veterans' health and well-being, which would integrate family and social support networks and other societal factors," Howard added.
Evidence from other recent studies of this population shows alcohol abuse plays a significant role in suicide risk, which suggests that more efforts to prevent alcohol and substance abuse in military veterans may be warranted, he said.
"Despite efforts in recent years to prevent suicide in military veterans the problem has continued to grow, which suggests that new approaches are needed," Howard said.
For the study, Howard's team looked at more than 8,200 suicides among veterans, comparing them with more than 562,000 U.S. adults in the general population.
The investigators found that between 2006 and 2020 suicide rates among veterans who suffered a TBI increased by 15% a year, compared with 14% per year among veterans without a TBI and 1% a year among the general population.
From 2019 to 2020, suicide rates per 100,000 people increased from 80 to 90 for veterans with a TBI and from 50 to 57 for veterans without a TBI, but it did not change in the general population, the researchers noted.
The report was published online Aug. 28 in JAMA Neurology.
"A consequence of TBI is you're more likely to develop a mental health disorder or struggle with addiction or substance use disorder," said Rachel Adams, a research associate professor in the department of health law, policy and management at Boston University's School of Public Health.
Veterans are at high risk in general for substance use disorder, she said. "If you add on exposure to TBI, veterans are at even higher risk. So, it's sort of a combination of exposures that I think are coming together for people in this population," she explained.
The suicide rates among veterans reflect the general increase in suicide and substance abuse plaguing the nation, Adams said.
"It is coinciding with the opioid and alcohol epidemic in our country," she said. "The alcohol crisis is sort of less focused on but I think we have seen increases in alcohol-related harms and deaths over this time period as well. So, I think these are coming together and impacting the veteran population more specifically than the civilian population."
Adams thinks more outreach to veterans is needed, not only by the Veterans Administration (VA) but by other health care providers. She pointed out that many recent veterans don't get their health care through the VA.
She noted that people in a crisis can call 988 and if they are veterans they can connect with the Veterans Crisis Line.
"That's a great immediate resource for people struggling," Adams said, but helping veterans is not just the job of the VA.
"We need to support each other," Adams said. "Our country, our community has a responsibility to support people who served our nation and we need to collectively provide more support to this population to feel less isolated and alone," Adams said. "That's not just the responsibility of the VA but all of us need to do a better job including our health care system and our communities."
More information
For more on veterans' suicide, head to the Veterans Crisis Line.
SOURCES: Jeffrey Howard, PhD, department of public health, University of Texas at San Antonio; Rachel Adams, PhD, MPH, research associate professor, department of health law, policy and management, Boston University School of Public Health; JAMA Neurology, Aug, 28, 2023, online

